How Inclusive Support Transforms the Recovery Journey
Recovery looks different for everyone. Each person brings a mix of experiences, beliefs, and personal challenges that shape the path forward. When support is inclusive, people feel seen rather than managed. They get to rebuild trust in themselves and others. Recovery becomes a shared process instead of an isolated effort.
Inclusive support in addiction recovery isn’t a specialised service or a single method. It’s a mindset built into every part of treatment: how people are spoken to, what kind of space they walk into, and how they’re allowed to express themselves. That sense of belonging can completely change how someone moves through the recovery process.
Why Inclusion Matters in Recovery
Addiction treatment often asks people to confront pain, guilt, or fear. Doing that in an environment that feels unwelcoming or judgmental makes progress harder. When people feel misunderstood, they may pull back or leave before they get what they came for.
Inclusive support creates psychological safety. It respects cultural background, sexual orientation, gender identity, age, ability, and spiritual belief. It acknowledges that no one recovers in the same way. A person who feels recognised can focus on healing instead of protecting themselves from bias or discomfort.
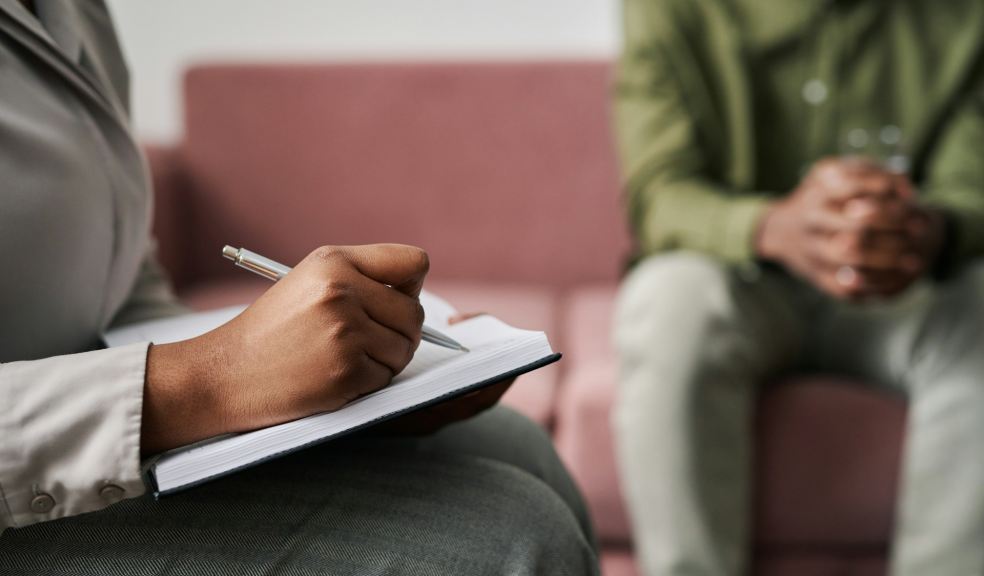
Programs that make inclusion a priority tend to foster trust faster. Clients talk more openly about what led to their substance use and what still triggers it. That honesty gives professionals the context they need to tailor care, which can strengthen long-term engagement.
How Inclusive Care Shapes Treatment
In addiction recovery, inclusion takes practical form through the people, the language, and the policies that guide care. Treatment centres that identify as LGBTQ-friendly recovery programs, for example, commit to using affirming language and building an environment where identity isn’t questioned or minimised. That kind of openness signals to everyone that differences are respected.
Inclusive care may look like offering single-gender or mixed-gender therapy options, adjusting communication styles, or making space for different cultural expressions of healing. It’s also reflected in staffing. Teams that mirror the diversity of clients create more trust and less distance. Representation helps normalise difference, which can break the pattern of silence and shame that often fuels addiction.
When inclusivity shapes the foundation of substance abuse treatment, clients experience fewer barriers to honesty. They can focus their effort on recovery rather than defence. That shift helps build resilience and reduces the sense of isolation that often drives relapse.
The Human Side of Connection
Support isn’t just about structured therapy sessions. It lives in the small moments: how someone greets a client in the morning, how they respond when emotions rise, how they hold space for grief or anger. Inclusive recovery practices turn those moments into anchors for trust.
Many people in treatment have spent years feeling outside of social circles or family systems. Recognising and respecting their story validates that pain without glorifying it. When people see they’re accepted, they’re more willing to take responsibility for their actions and choices. They begin to reconnect with themselves, which is a quiet but powerful step in healing.
In this kind of environment, recovery becomes more than symptom management. It becomes a chance to rebuild a sense of belonging. That matters as much as any medication, therapy, or structured plan.
Building Inclusive Systems in Practice
Creating inclusive recovery programs requires continuous effort. It involves revisiting policies, training staff, and listening to feedback. Language changes, social awareness evolves, and treatment must move with it.
Programs can start small. Providing resources in multiple languages, respecting dietary or spiritual needs, and offering both individual and group formats can make care more accessible. Support groups built around shared identity, such as cultural, gender, or faith-based communities, give clients a familiar anchor during recovery.
Community organisations often bridge the gap between formal treatment and real life. They help people maintain support systems in sobriety once residential care ends. Having networks that feel authentic and inclusive can reduce the risk of relapse and increase participation in continuing care.
Mental Health and Inclusive Recovery
Addiction often intersects with other challenges like anxiety, trauma, or depression. Addressing these issues alongside substance use requires sensitivity and skill. Inclusive care integrates mental illness treatment without separating it from addiction support. People don’t have to divide themselves into categories to get help.
Programs that combine therapy, medication, and peer connection treat the person as a whole. Approaches like talking therapy, Intensive outpatient programs, and 12 step programs work best when clients feel they can speak freely. That sense of safety reduces shame and encourages honesty. When care teams understand the cultural and personal factors behind addiction, they can respond in ways that feel respectful instead of prescriptive.
Inclusivity also supports mental health management during early sobriety. It recognises that recovery isn’t just about stopping substance use but learning to handle stress, rebuild routines, and reconnect with others.
The Role of Environment and Access
Physical and social environments can reinforce inclusion or undermine it. A residential drug rehab that reflects community diversity sends a message of belonging. So does offering multiple treatment options such as medical detox, therapy, and addiction treatment plans tailored to individual needs.
Inclusivity also means acknowledging external pressures. Many people entering recovery face legal problems, family strain, or job loss. Treatment that takes those realities into account helps people rebuild without shame. When programs collaborate with community organisations, faith community leaders, or self-help groups, they extend the circle of care beyond the clinic.
These connections turn recovery from a medical event into a community response. Support continues outside formal treatment, where most of life happens.
Tools for Sustainable Recovery
Inclusion doesn’t stop at treatment. Long-term recovery depends on practical habits and ongoing support. Structured routines like maintaining a gratitude journal, attending Alcoholics Anonymous meetings, or joining peer-led groups can reinforce stability. Building support networks grounded in empathy keeps recovery social instead of solitary.
Skills training also helps. Learning life skills such as managing money, setting boundaries, or handling conflict prepares people to live full lives beyond treatment. Recovery then feels less like survival and more like participation.
A strong network acts as natural relapse prevention. People who feel accepted and connected are more likely to reach out before things spiral. Inclusion gives those networks depth and durability.
Final Words
Addiction recovery isn’t a straight line, and it rarely fits into a single program model. What holds it together is connection, the kind that respects each person’s history, identity, and hopes. Inclusive support doesn’t guarantee an easy path, but it builds an environment where honesty and healing can take root.
When people are treated as whole human beings, recovery becomes possible on their own terms. That’s what inclusive care really means: an open invitation to heal without having to leave parts of yourself at the door.