Plymouth baby is first to receive life-changing surgery
A Plymouth baby has become the first in the UK to receive life-changing surgery for spina bifida while still in the womb.
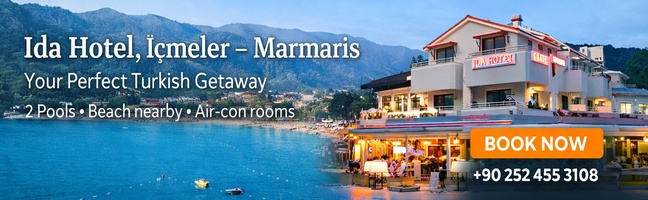
Sat with her doting parents and smiling at the camera, eleven week old baby Frankie Lavis, is still totally unaware of the revolutionary operation she had before she was even born.
In May this year, Gina Beddoe, 35, and her partner Dan Lavis, 39, from Devonport in Plymouth, came up to the Maternity Unit at Derriford Hospital, Plymouth for a 19 week scan. It was at this appointment they were told that it looked as though their unborn baby had spina bifida, a fault in the development of the spinal cord and surrounding bones, which leaves a gap or split in the spine.
The following day they returned for an appointment with Consultant in Fetomaternal Medicine, Dr Ross Welch, who confirmed that their baby did have spina bifida.
“The next day we came back in and met with Dr Welch and that’s when he said it was definitely spina bifida and that it looked quite extensive,” explains Gina. “The options given at that time were not to continue [with the pregnancy] or to repair it afterwards. He sent us away to think about, obviously it was quite a shock.”
For Gina and Dan the decision to keep their baby was immediate. Dan said: “We didn’t even have to ask each other whether we would continue with the pregnancy.”
“For us, it was the right decision,” added Gina. “We have very good support from friends and family and as our other children are seven and 16 we felt we could cope with another child with extra needs. But everyone’s circumstances are different. Everyone makes the decision that is right for them, this was our right decision.”
Image of baby FrankieAt home after their appointment, the couple looked up spina bifida online and that was where they learned about fetal spina bifida repair before birth. “The first thing I did; I looked online,” Gina said. “I only found positive things about it though on there and I read about the in utero surgery. So when we came back in to discuss the options I asked about the surgery and was told that it wasn’t done in the UK.
“Dr Welch said that he could look into it for us if that was the route we wished to take. At that point, about 20 weeks I still wasn’t 100% sure. It is big surgery to go through and Dr Welch explained that it was extensive surgery, not an easy five minute thing.”
The couple thought about it for a further couple of weeks and after receiving counselling and speaking to family, friends and Shine (the charity for spina bifida), Gina and Dan decided that the repair whilst in utero would offer their baby a better chance of reduced disability than having the surgery after birth, which is the standard treatment for babies with spina bifida.
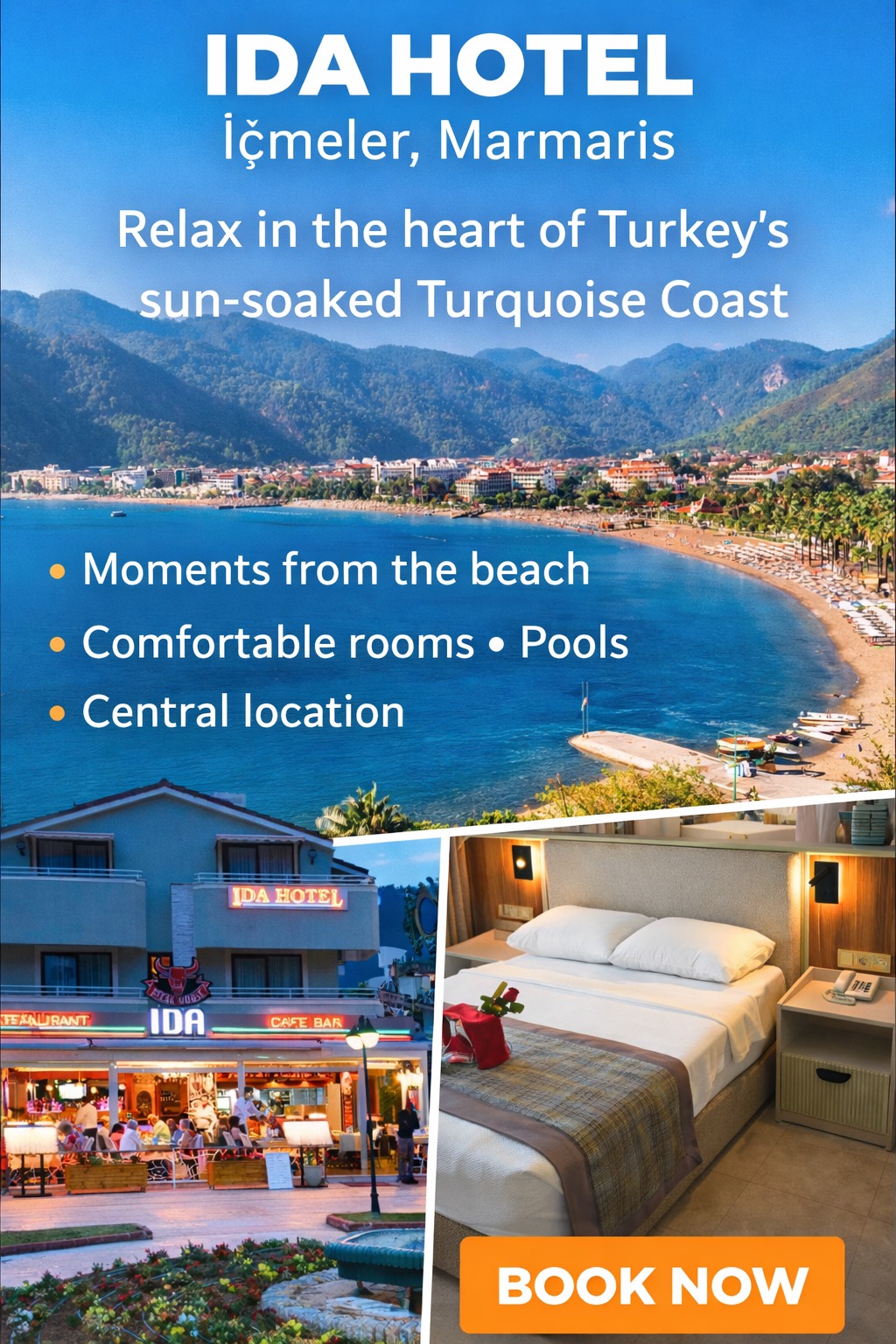
At 22 weeks pregnant, Gina expressed to Dr Welch and his team that she wished to go ahead with the surgery and so Dr Welch, a former president of the International Fetal Medicine and Surgery Society, contacted Professor Jan Deprest in Belguim, who leads one of only four centres in Europe that performs the operation.
This type of surgery needs to be performed before 26 weeks so arrangements were quickly made by the Derriford team to ensure the operation could take place. Fortunately, the operation was approved by NHS European Cross Border Funding agency within 30 minutes of the request being made and the couple were able to meet the costs of their flights and accommodation.
Image of Gina, Frankie, Dan and the fetal medicine team at Derriford Hospital“We went across to Belgium when I was 24 weeks pregnant,” explains Gina. “I nearly changed my mind; I just felt it was too much. Our flight was delayed which didn’t help matters and once we got there it was just test after test. The team over there were fantastic and they spoke the best English they could but we couldn’t read the signs; it was so overwhelming. We got back to the room and I just said ‘I can’t do this, I just want to go home’.
“Then Ross, Sharon and Llinos from Derriford, came out and I also spoke to a mum in the Netherlands who had had the surgery there and showed me her video and that put me at ease a bit and I started to see the surgery as an opportunity.”
The open surgery was performed in June and took two hours and involved more than 20 surgical staff. To access the baby’s spinal lesion, the surgeon had to cut through Gina’s abdomen, uterus and into the amniotic sac that held the baby.
“It depends on where baby is and where the lesion is,” Dr Welch explains. “The first thing the surgical team do is turn baby into a good position, if they can. In this situation, baby was. Guided by ultrasound, they put in sutures and then cut down carefully through the uterus. One of the main difficulties with open fetal surgery is ensuring the membranes and embryotic sac doesn’t move away from the uterine wall so they have to staple it into place.”
During this procedure one of the surgical team has to hold baby so their back is out of the sac but they remain face down in the fluid, which is continuously topped up throughout the procedure.
“If baby gets cold or dry then the reflexes can trigger and baby will start to breathe and that of course reverses the whole fetal circulation into an adult circulation. If that happens then there’s no going back.
At 24 weeks that was not an outcome we wanted,” said Dr Welch.
The repair was carried out and in this case, due to the size of the opening of the spine the surgical team had to use an artificial skin substitute to cover the wound, which skin will later grow over.
Gina was in hospital in Belgium for ten days and when she returned home she was on strict orders to reduce activities and rest as much as possible. She was also seeing Dr Welch and his team on a weekly basis. As delivery must be by caesarean section following surgery, Gina was booked in for an elective section at 36 weeks pregnant, for the beginning of September.
However, a week before her planned date, Gina’s waters broke and baby Frankie was delivered at Derriford Hospital. “I was booked in for 36 weeks but she [Frankie] decided to come a week earlier!” smiled Gina. “I did keep saying she wanted to be an August baby. She was very keen to come early and we had her here.
“We wanted her to be born here, we could have had her in a surgical hospital, in case she needed a shunt but we wanted her born here. We wanted her where everyone who had been with us all the way through was. We were more confident with that.”
Frankie did have a skin graft from her thigh a few days after delivery, to cover the artificial skin patch and a shunt fitted when she was three weeks old after fluid started to build up in her brain. But Gina and Dan are hopeful that the prenatal surgical repair has helped secure a more independent future for their daughter.
Gina is the first woman in the UK to be funded by the NHS to have this procedure. “I strongly believe that if we hadn’t been at Derriford Hospital we would never have got the option of the surgery,” said Gina.
“We know that she’s the first baby in the UK to have the surgery and we also know that there are many more babies who could qualify for the surgery but it’s not being offered as an option at the moment. Maybe because it’s abroad, maybe because it’s a big operation and commitment but we knew it was the right option for us. It might not be for everyone, and I completely understand that, for us though it was the right thing. The proof is in what she can do now.”
More than two months later, Gina describes that whilst Frankie has reflux and they need to be aware of her shunt, she is just like any other baby.
“The only difference being is that she likes to sleep on her belly,” Gina adds. “When she was first born she couldn’t go on her back because of the skin graft so she’s now got a preference for that. Apart from that, if you saw her, you wouldn’t know. There’s no outward sign that she has spina bifida and there’s certainly no sign that it’s as large as what it is.”
It’s too early to know if she might walk but Frankie has sensation in the underside of her foot and according to Dr Welch, the strength in her legs is normal. The couple will have to wait to see if Frankie will require any neurosurgery or physiotherapy and also how she will meet targets, such as crawling, but for now everything looks fine.
“There was no guarantee that the surgery would be helpful. It is high risk,” said Gina. “You have to have bed rest afterwards and it was quite a stressful time and you don’t know the outcome. We were lucky. Frankie is perfect.”